In its 10th season of connecting people with health insurance Affordable Healthcare Act enrollment is seeing changing premiums and an estimated record-breaking application period, thanks in part to the Medicaid unwinding process in which states -- including Florida -- are redetermining Medicaid eligibility for millions of people, estimates show.
In Central Florida, navigators with the Primary Care Access Network (PCAN) already have appointments set up for those seeking coverage Wednesday — the first day of ACA, or Obamacare's open enrollment.
"These navigators are booked for days, but of course, they have availability for anybody that would come through our appointment system, either through our website or through our portal," said Rebecca Sagoya, director of PCAN.
How to get in touch with a navigator.
Exploring the nuances of the Marketplace can be complicated for the uninitiated, Sayago said. She highly recommends getting in touch with a navigator.
"Some people think that, okay, I'm savvy enough that I can do this on my own, it's just renewing my plan. I'm going to choose the same features, the same insurance carrier and it's not a good idea. We don't suggest that because there are some changes that they're not going to know ahead of time," Sayago said.
Marketplace navigators can assist in finding a plan for free. PCAN has 17 healthcare navigators serving Orange, Seminole, Lake, and Osceola counties. They're available over the phone or via Zoom call. Navigator help is available in several different languages including Vietnamese, Spanish, Ukrainian, Russian, Portuguese, and Creole languages.
You can schedule an appointment with a navigator by visiting Coveringcfl.net or by calling 1-877-564-5031.
The Marketplace process takes about two to three hours for new enrollees and about 45 minutes for those renewing
Open Enrollment is growing
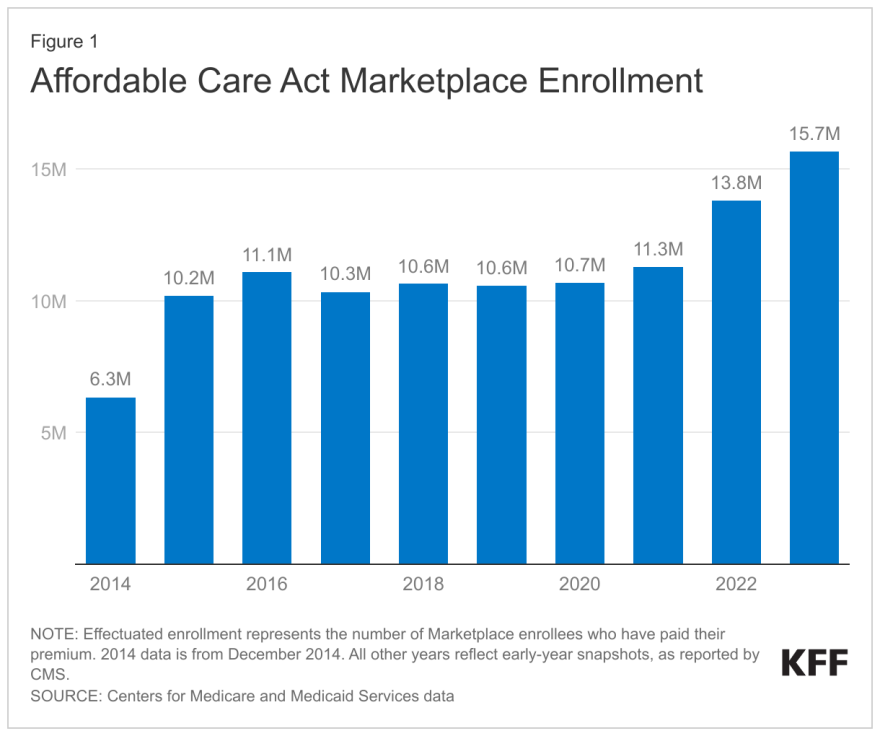
Between 2022 and 2023, the number of those on ACA plans increased from 13.8 million to 15.7 million, according to the Kaiser Family Foundation. KFF estimates that the 2024 enrollment period will likely set another record for the fourth year in a row, as Medicaid unwinding continues.
The redetermination process is expected to terminate 15 million from Medicaid. About 51% of those who lost coverage as of last April in Florida lost it for "procedural reasons" meaning their termination was due to the fact that no contact could be made between an individual and the Florida Department of Children and Families.
A special enrollment period exists outside of the open enrollment period for those found to be ineligible for Medicaid during the unwinding process. PCAN is also available for those seeking coverage within 60 days from the date they were terminated from Medicaid.
“The benefits that we have at PCAN are very unique because our navigators are run around the year helping during special enrollment period during the Medicaid unwinding, and now do an open enrollment,” Sayago said.
However, those terminated from Medicaid may not qualify for an ACA plan due to not meeting poverty-line standards or income guidelines, in which case they would be rerouted to a federally qualified health center, so so they can have access to care, Sayago said.
Premiums are growing, but don't necessarily worry
To make matters more complicated, low-cost premiums are expected to rise.
Unsubsidized premiums are rising by an average of 5% in 2024 for the second-lowest-cost silver plan, and 6% for the lowest-cost bronze plans, according to KFF. The increase is due to rising prices paid to healthcare providers, driven partly by inflation. However, a byproduct of the Inflation Reduction Act is its enhancement of subsidies, making the vast majority of Marketplace shoppers eligible for financial help with the cost of coverage, according to KFF.
Sayago is concerned that folks may attribute the rise solely to inflation and decide to get off their current plan because of the increase, but it's not that simple.
"They're afraid that they're going to get hit with a, you know, higher premium or higher deductibles and co-pays. And our message is across the board is making sure that people don't assume that immediately," she said. "Some bronze plans and some silver plans are going to have some changes. Some are going to benefit the consumer. If they're already enrolled in that plan, it's going to benefit them because it's going to get them a lower premium and in some instances, it could change a little bit of their benefits under their current plan."
Sayago said available plans may differ if income or residence has changed over the year. Giving her one more reason to push people into seeking navigator help.
"They have navigators available. It's free assistance to the community. So why not take advantage of it?" she said.






